As a single mother returning to college, Carla D’Agostino-Vigil enrolled in Medicaid and used government-run health insurance to undergo “life-saving” therapy. So when she graduated and started her own mental health consulting firm in Westminster, D’Agostino-Vigil was adamant that she would open her doors to Medicaid patients.
“When it was my turn, I felt very strongly involved,” she said. “The way things turned out, my heart is broken.”
Two years after opening his practice, D’Agostino-Vigil is among the last Colorado healthcare providers to leave the Medicaid program. Almost half of Ignite Counseling Colorado’s 175 patients are on Medicaid, and during a six-month transition phase, D’Agostino-Vigil will “try like hell” to find other counselors who will take them. If that doesn’t work, she intends to continue helping some pro bono.
His list of reasons is long. There was the 20% drop in rates in 2020, just before an increase in mental health care needs due to the days of isolation from the pandemic. There were threat letters warning her that she was “abusing” a billing code – the code for a full hour of therapy – and that she should instead see patients for 30- or 45-minute sessions.
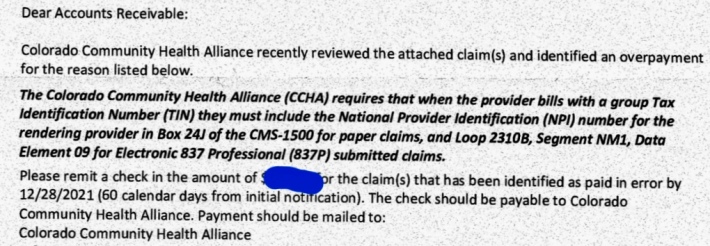
But what drove D’Agostino-Vigil, one of the only obsessive-compulsive disorder specialists to take Medicaid in Colorado, to boil over was a “recovery” advisory received by his practice and nearly 200 others in the country. Colorado this fall. The letter said that due to incorrectly filed claims, providers would have to pay hundreds or thousands of dollars to the agency – called the Colorado Community Health Alliance – that makes their payments. In some cases, the payback amounts totaled $ 17,000 or $ 18,000 for a single mental health therapist in private practice.
The letters, copies of which have been reviewed by the Colorado Sun, warn that suppliers have 60 days to pay or that the management agency may withhold future payments.
The debacle is the latest headache for Medicaid providers who for years have complained about redundant paperwork and cluttered bureaucracy. And in this case, it’s not that therapists and counselors have been overpaid – they are being asked to reimburse for the services they provided in the previous two years, all because of a number d. ‘identification of a supplier who was not included in the complaints.
Several behavioral health clinicians told The Sun that they included the provider ID number. It was the computer system used by their payer, the Colorado Community Health Alliance, which is owned by private insurance giant Anthem, that erased the ID numbers from its claims, believing they were unnecessary.
The Health Alliance, which is the middleman between providers and the state Medicaid program, realized its mistake two years ago and began warning treatment practices in March 2020 that they should resubmit demands, said spokeswoman Colleen Daywalt. The vendor number is required by federal and state law. So when the alliance discovered the problem in July 2019, the agency began patching its software system to include the number on its claim forms. The issue was resolved in October 2020, Daywalt said.
Colorado Community Health Alliance, which is the payer for behavioral health care providers in Boulder, Broomfield, Clear Creek, El Paso, Gilpin, Jefferson, Park, and Teller counties, began notifying providers in March 2020 that claims filed over a two-year period were exhausted. of compliance. But many of the alliance’s 1,175 vendors took no action, overwhelmed by the task of resubmitting hundreds of requests.
A therapist who saw a client every week over those two years would have filed around 104 claims – and that’s just for one patient.
The health alliance last month sent out 199 letters asking for ‘clawback’ payments, triggering panic and a storm of complaints, including to a private Facebook group where therapists and counselors speak out about frustrations of Medicaid.
Daywalt said the health alliance did not intend to recover payments, only to comply with federal and state laws. It would not say the total amount of money involved in non-compliance claims or the range of recovery amounts sent to suppliers.
But several therapists reached out to The Sun about the payment debacle and shared their clawback amounts.
Allison Harvey, who works at a small-group practice in Arvada, said the healthcare alliance is asking for $ 7,000 for 74 claims in 2020. “The problem is, we have submitted all of these claims correctly with all the necessary information. on payment, “she said. noted. “The data is deleted sometime after the complaints leave us. Our group, like all providers who choose to serve Medicaid clients, simply wants to be paid for the work we do with this important clientele.
Christia Young, of Badass Therapy in Brighton, has been asked to reimburse $ 7,200. Now Young has stopped taking Medicaid patients through the Colorado Community Health Alliance. Even before the last issue of claims, she was spending 80% of her time processing Medicaid claims because the health alliance “repeatedly verified” her claims, she said.
And Sarah Carlson, a licensed marriage and family therapist who has accepted Medicaid for 13 years, is quitting her Medicaid contract with the Alliance for Health starting next month. She founded the Parent-Child Interaction Center, one of the largest Medicaid-accepting group practices in Larimer, Weld and Boulder counties.
Carlson said she has been fighting for years over claims with the alliance for health. The agency owes her thousands of dollars in past claims and is now asking about $ 6,000 in clawback on payments she received for 2020 and 2021, she said.
“I like the way they can find the claims all of a sudden when they want to get the money back, but somehow manage to not have the others in their files?” Carlson said. “It’s a game, and it’s disgusting. Especially during the pandemic when the needs have skyrocketed. “
Carlson said she would have a hard time paying rent for her office serving Medicaid clients and that she needed to subsidize Medicaid patients with those who have private insurance. “Unfortunately, it will be my underserved clients who will suffer, but I cannot continue this way,” she said.
The Colorado Department of Health Care Policy and Funding, which manages the Medicaid program and contracts with the Colorado Community Health Alliance to distribute payments to providers, said providers were warned of the error. complaint via several newsletters and meetings in 2020 and 2021.
“While we understand this is frustrating for vendors, vendors and payers are responsible for submitting and processing compliant claims,” said an emailed statement from department spokesperson Marc Williams. “Our contractor identified a system problem preventing this and corrected the problem. They have given vendors 21 months to submit corrected claims, which they are still able to do before clawbacks take effect. “
While some providers terminate their Medicaid contracts this fall, the number of behavioral health care providers taking Medicaid has increased statewide over the past year, Williams said. Network practitioners reached 8,371 in June, up from 6,029 in April 2020, he said.
But Stephanie Farrell, CEO of Left Hand Management, a consultancy group that helps behavioral health care offices across the state with billing and training, said the alliance for health caused the problem and should have to solve it – without putting the burden on the small counseling centers. The Colorado Community Health Alliance should pay the consequences, Farrell said, including any potential federal fines for submitting incomplete documents.
“It’s just a matter of the office. A data problem, ”she said. “Can’t they say, Let’s call it a mulligan?” ” ![]()
This is the latest example of what Farrell says is a messed up system in which the people providing mental health care have no voice and are buried under mountains of paperwork. She blames the organizational structure and the contractors who make the payment.
“It’s the wild Wild West,” she says. “They just do what they want and they crush the suppliers in the process.”

 HS Alliance
HS Alliance